
New discoveries: 231 research publications sharing new knowledge on brain tumours; 53 new research tools and methods, and 10 new research databases to enable global collaboration and efficiency
Turning discoveries into better treatment: 11 new medical products, interventions and clinical trials; 5 software and technical products
Stimulating more research: 87 research collaborations and partnerships plus £89m of additional funding into brain tumours from others

Invest £20 million from 2015 to 2020, later increased to £32.5 million

Invested £38 million up to March 2020




We cannot detail all of the research impact outlined above, but below is a case study of our pioneering research and further examples to explore.
Across three institutions and led by Dr David Jones, an expert in molecular biology, The Everest Centre is a ground-breaking international initiative established in 2017 to propel our understanding and improve treatment of paediatric low grade brain tumours.
So far, The Everest Centre team have:

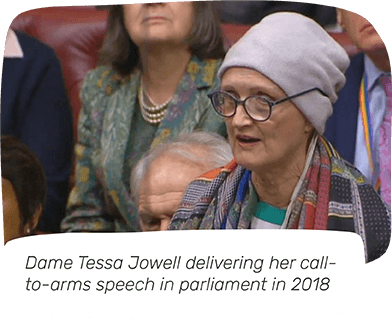
A highlight: We helped found, and have invested £2.8m in, The Tessa Jowell BRAIN MATRIX, a pioneering clinical study and biobank, providing a platform to trial precision medicines.
The BRAIN MATRIX, running from 2019 to 2023, provides a common infrastructure across at least ten key treatment centres in the UK, with all participants starting by having their tumour tested for its biological and genetic profile. This platform can then be used for additional clinical trials, while not being unduly expensive, meaning more people can be offered potentially beneficial drugs.
Through the implementation of BRAIN MATRIX, we will work to deliver routine biobanking for adults with a brain tumour, to further accelerate research and improve both survival and quality of life for those affected.

A highlight: Our funded research has created a tool to predict meningioma recurrence.
Dr Gelareh Zadeh and her team analysed over 500 meningioma samples to find DNA changes that result in tumour growth. Combined with clinical images, this molecular data gives a five-year recurrence score, from which a software tool has been developed.
This tool is now freely available to doctors globally and helps to predict the outcome for those affected by meningiomas, define appropriate treatments and ultimately reduce the harm caused by brain tumours.
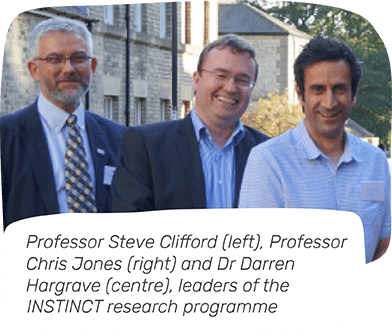
A highlight: Our INSTINCT research programme is a collaborative network to beat aggressive childhood brain tumours.
The network, led by Professor Steve Clifford, Professor Chris Jones and Dr Darren Hargrave, brings together world-class researchers in genetics, biochemistry and drug discovery to understand some of the most lethal childhood brain tumours and translate this knowledge into the clinic. So far, the team have:

A highlight: Initiatives such as the Brain Race have catalysed progress towards finding new, effective treatments for brain tumours.
In collaboration with Resonance Philanthropies and the Center of Advancing Innovation (CAI), The Brain Race was an open innovation contest and opportunity for 15 start-up companies to launch promising to high-impact solutions to defeat brain tumours.
With access to CAI’s White House-accredited accelerator training programme, including technology commercialisation classes and expert advice, 124 teams were hosted and the 15 winners were announced in April 2020.
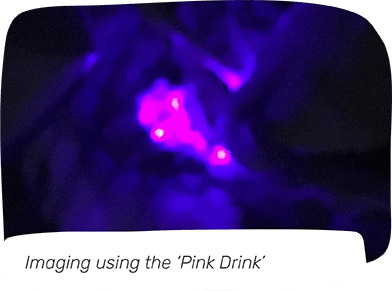
A highlight: Through activities such as campaigning for the ‘Pink Drink’ to be accessible throughout the UK, we have enhanced care and quality of life in meaningful and practical ways, ensuring that those affected receive the best treatment, irrespective of postcode.
For people with a high grade glioma, surgery is the major line of treatment. 5-AminoLevulinic Acid (5-ALA, or the ‘Pink Drink’) is a pink dye that helps neurosurgeons to achieve a higher percentage of successful tumour removal, which is associated with longer survival. With 5-ALA, the whole tumour is removed in 70.5% cases, up from around 30% without. With total removal of the tumour, recurrence is delayed and survival is significantly improved.
Previously, access to the Pink Drink depended on postcode, but as a result of our research and many years of campaigning, 5-ALA was rolled out across all 27 neurosurgery units in the UK in 2018, and recommended by NICE as part of their updated guidelines for brain tumours.