Proton beam therapy for brain tumours
Proton beam therapy is a specialised form of radiotherapy that involves directing a beam of protons (energised sub-atomic particles) specifically at the tumour.
On this page, we’ll cover:
- What is proton beam therapy?
- What is the difference between proton beam therapy and radiotherapy?
- Can I have proton beam therapy for a brain tumour?
- What happens if proton beam therapy is suitable?
- How is proton beam therapy given?
- What are the side-effects?
- If proton beam therapy doesn’t work
What is proton beam therapy?
Proton beam therapy (PBT) is a type of radiotherapy used for cancer treatment. It uses beams of ‘protons’ (energised particles), instead of beams of X-rays (‘photons’), that are used in conventional radiotherapy. It is more targeted than conventional radiotherapy so does less damage to the healthy tissue around the tumour and in the rest of the brain.
A machine (called a cyclotron or particle accelerator) speeds up the protons causing them to gain energy. Once a high level of energy is reached the protons are then beamed out of the machine and guided by magnets towards the tumour.
Protons accurately release most of their cell-killing energy at a particular depth in tissue. This depth can be varied by the medical team who programme the PBT machine. The beam of protons can be set up to stop once it has ‘hit’ the tumour cells (and travelled for a safe margin past the tumour to capture any tumour cells beyond the visible edge of the tumour).
This means that proton beam therapy destroys the tumour cells whilst not affecting so many of the surrounding cells. In particular, PBT delivers very little radiotherapy in a path through the rest of the brain on the other side of the tumour, unlike other high energy beams (X-rays) used in conventional radiotherapy.
What is the difference between proton beam therapy and conventional radiotherapy?
Radiotherapy
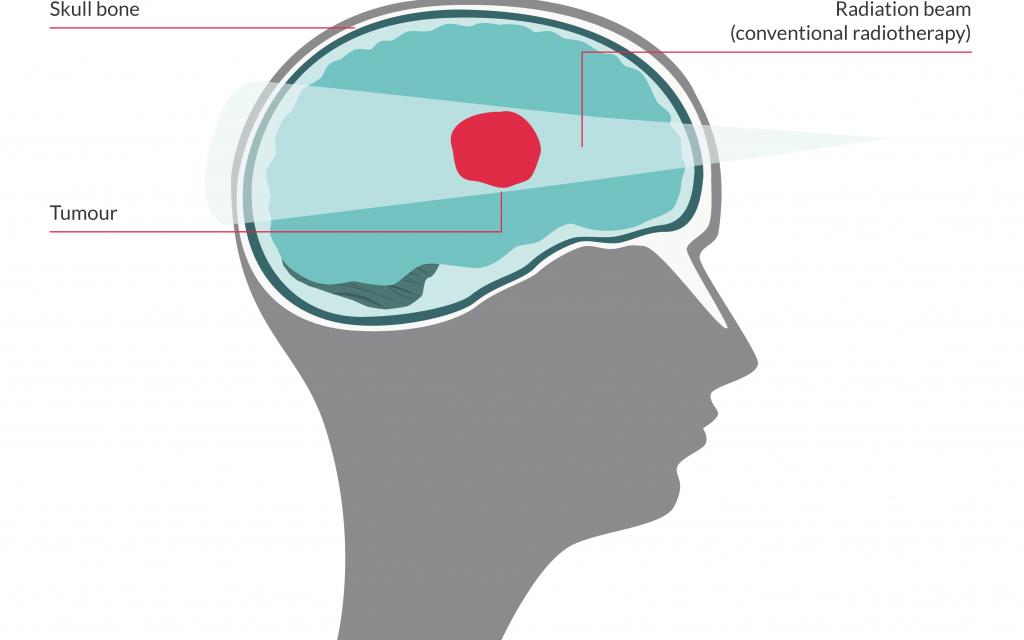
With conventional radiotherapy, the beams of X-rays are carefully planned to deliver most of their energy within the tumour, whilst avoiding as much healthy brain tissue as possible.
However, the X-rays do also release some of their energy before they reach the tumour, and continue to release some after they have passed through the tumour and continue on through the brain to exit on the other side of the head.
This causes some damage to the normal, healthy cells in the path of the radiotherapy. But, normal brain cells are more able to repair themselves than tumour cells.
This initial damage to the normal cells, however, can cause side-effects in the short-term. Some of the damage may be unrepairable, leading to long-term effects.
Proton beam therapy
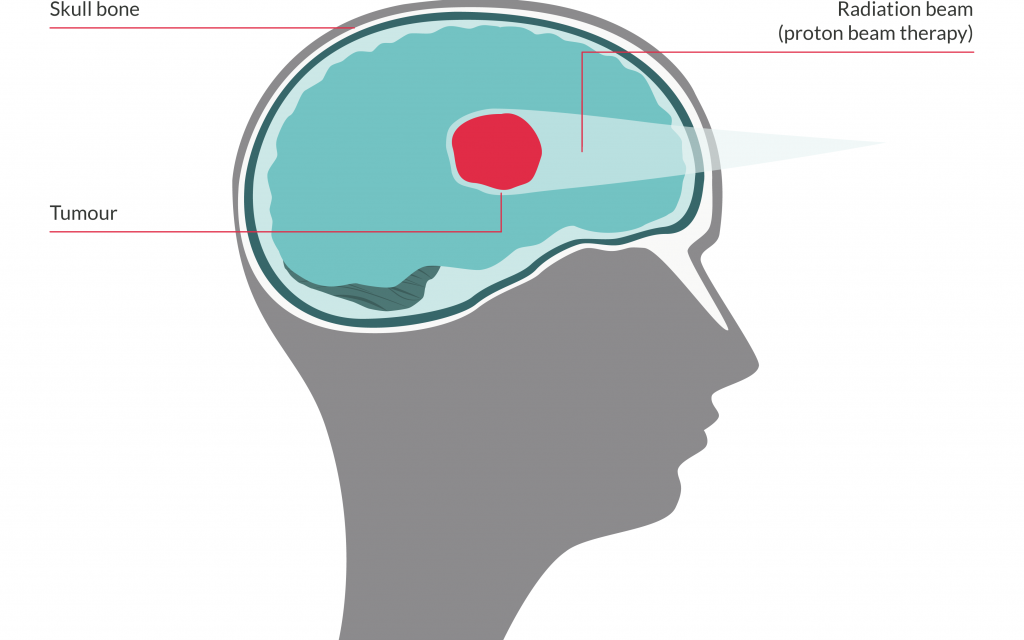
In PBT the beams of protons are also carefully planned to target most of their energy within the tumour.
But, by altering the beam energy, the beam can be designed so that the protons stop and release most of their energy accurately at a particular depth in the brain i.e. where the tumour is situated.
This means that although some of the energy will be released before they reach the tumour, the main radiation dose can be given to the tumour and very little is released the other side of the tumour.
As proton beam therapy is highly targeted towards the tumour, it means it is often possible to treat areas closer to very sensitive structures such as the spinal cord or optic nerve.
The beam is usually set up to travel a little way past the tumour to make sure it gets any tumour cells beyond the edge of the tumour that can’t be seen.
This means that fewer healthy cells nearby receive a dose of radiation. This is particularly important in children, whose brains are still developing.
The reduced damage to surrounding healthy tissue means the tumour can be given a higher dose of radiation.
Can I have proton beam therapy for a brain tumour?
Whether your child/you can have PBT depends on many factors, including:
-
PBT is not suitable for all types of brain tumour. It works best for smaller tumours and those where the edges are clearly defined.
It is also useful where the tumour is close to very important structures like the spinal cord or optic nerve, or when it is important to reduce the damage caused to surrounding normal tissue as much as possible e.g. brain tumours in young children whose brains are still developing.
There is a nationally approved list of tumour types that are suitable for referral.
With regards to brain tumours, these include:
Children, teenagers and young adults:
- ependymoma
- optic pathway and other selected low grade glioma
- craniopharyngioma
- pineal parenchymal tumours (not Pineoblastoma)
- base of skull and spinal chordoma
- base of skull chondrosarcoma
Adults:
- base of skull and spinal chordoma
- base of skull chondrosarcoma
Though not on the approved list, PBT has sometimes been used to treat medulloblastomas in children. However, diagnosis alone is not enough. PBT will only be given if it is thought it will give a significant advantage over conventional radiotherapy.
-
It is most important that PBT seamlessly links with surgery and chemotherapy. Disruption in the pathway, and the resulting delays, can lead to less intensive therapy and a reduction in tumour control. This could counteract any longer term benefits. This is particularly important in the treatment of high grade, ‘malignant’ brain tumours, such as medulloblastoma.
It is also important to note that referral abroad might delay the giving of radiotherapy for longer than the health professionals would advise.
It is also important to realise that:
- PBT is a relatively new therapy that is usually used for rare types of tumours. This means there is little evidence about its effectiveness compared to conventional radiotherapy, particularly about long-term side-effects.
- The way it works when it reaches the tumour is much the same as conventional radiotherapy.
- The quicker ‘stopping’ of the radiation in PBT means getting the target right is very important.
- It needs extra training and skill to work out the required depth and dosage of PBT.
- It is harder to check what is actually being treated during PBT treatment. Conventional radiotherapy can use imaging to check the accuracy of the treatment area, which is important when it’s close to critical structures like the spinal cord or optic nerve.
- People who travel to receive PBT often respond well, but they are ‘optimally chosen’ specifically because they are more likely to do well.
What happens if proton beam therapy is suitable?
If the Clinical Oncologist feels that PBT may be suitable for you/ your child, they will, with your agreement, refer your/your child’s case to the Proton Clinical Reference Panel (PCRP) of the UK Proton Overseas Programme for consideration. This is the same for patients from England, Wales, Scotland and Northern Ireland.
There is a strict set of criteria that a patient must meet for a referral for PBT to be made. Funding for treatment will not be approved outside these strict criteria. It is also unlikely that the treatment will be successful if these criteria are not filled.
Where can I receive PBT treatment for a brain tumour?
There are currently two NHS centres that provide proton beam therapy in the UK. One is The Christie NHS Foundation Trust in Manchester and the other is the UCLH (University College London Hospital) in London.
Unfortunately, other current UK proton beam therapy machines are low energy machines. This means they can’t deliver the protons at a high enough energy to reach the depth in the body where brain tumours are situated.
The NHS might refer appropriate cases to approved treatment centres in Europe (Germany or Switzerland) or the USA. Children tend to go to Essen in Germany.
There are other (private) centres overseas, but people/parents should be aware that these can be expensive, may not have sufficiently trained staff and often don’t offer other treatments, such as chemotherapy, which may be required alongside the PBT. The lack of these additional treatments could have an effect on the overall effectiveness of the treatment.
When it comes to private centres, it’s also not clear:
- How many NHS patients will be able to use these private facilities
- How easy it will be to integrate this treatment with the patient’s overall care, which will remain with the main treating hospital (this is particularly important in the treatment of children)
- Whether patients treated there will be able to take part in clinical trials.
Will I have to pay for PBT?
Not if you are approved for treatment by the PCRP. The NHS will cover the cost of PBT treatment at approved treatment centres, whether in the UK or in the USA and Switzerland. If you are sent abroad, it will also fund economy travel and approved accommodation for the patient and one to two carer(s)/parent(s) accompanying them.
The accommodation has to be approved by the treatment centre. The number of carers/parents funded will depend on the age of the patient. If aged over 16 years, only one carer/parent will be funded, except in exceptional circumstances.
The NHS will NOT fund any meals or refreshments, nor any upgrades to travel or accommodation.
If you live in England, NHS England pays for treatment and your travel and accommodation costs.
If you live in Scotland, NHS England will pay for treatment, plus your travel and accommodation costs, then claim the money back from NHS Scotland.
If you live in Wales or Northern Ireland, your consultant will contact your local health board/trust directly about funding for treatment, travel and accommodation costs.
If you need help with associated essential costs not covered by the NHS, contact our Support team about sources of grants and other financial help that may be available. Also, your local neuro-oncology centre may have access to charitable funding.
Take a look at the NHS page on proton beam therapy for guides on getting proton beam therapy overseas.
How is proton beam therapy given?
The procedure for giving PBT is very similar to conventional radiotherapy.
In preparation:
There will be several planning appointments at the treatment centre before you/your child starts PBT. These include:
- scans to plan the treatment and programme the machine accurately
- a radiotherapy mask. This will be custom-made to keep your child’s/ your head still and in position during the PBT sessions. The mask will be made from a mouldable sheet, which is soaked in warm water and laid on your face. It will feel a bit like having a warm flannel across your face. You will wear the mask during PBT sessions to help hold you in position and keep you still. Some centres use tiny beads implanted under the skull (under anaesthesia) to act as pinpoints to ensure the head is located in the same place instead of a mask.
- the chance to discuss the treatment, what to expect and any possible side-effects.
After these appointments there is usually a two week gap whilst
the treatment plan is calculated and prepared specifically for
you/your child.
The proton beam therapy procedure:
- Your child or you will lie on a treatment couch, and the mask will be placed over their/your face and attached to the couch. You will be positioned correctly. Young children may need to have a general anaesthetic each day of treatment to make sure they stay still.
- Before the PBT begins, the radiotherapy team will leave the room, but they can still see and hear your child or you. You will not be allowed to stay in the room with your child.
- A machine called a cyclotron accelerates the protons to high energies. The protons then exit the machine, guided by magnets, towards the tumour.
- Once at the site of the tumour, the protons deposit their energy, destroying the tumour cells.
- After treatment, the team will re-enter the room and help take off the mask.
You will then usually be able to go straight home.
The treatment generally only lasts one minute, but with the positioning and adjustments, the session is likely to be about 20 minutes.
It is usually given daily (Monday to Friday) for up to 5-7 weeks. This depends on your child’s/your tumour type and grade.
You will need to be away from home for at least 8 – 10 weeks.
-
No, PBT is usually given as an outpatient treatment, which means you do not need to stay in hospital.
Occasionally, you /your child may need to stay in hospital. For example, if you/your child have side-effects that need inpatient care, or if you/your child need inpatient chemotherapy alongside the PBT.
It is worth bearing in mind, however, that brain tumour patients are usually referred to Switzerland or the USA for PBT, which can mean substantial time away from home.
-
The PBT itself shouldn’t cause any discomfort, but you may experience some temporary unwanted side-effects following the treatment.
What are the side-effects of PBT?
The side-effects of proton beam therapy are likely to be fewer than with conventional radiotherapy. But, your child’s or your side-effects will depend on the size of the dose of PBT you had and whether you are having any other treatment, such as chemotherapy.
If proton beam therapy doesn’t work
Although your child’s treatment plan will be carefully developed by healthcare professionals to be as effective as possible while having the fewest risks or side-effects, sometimes proton beam therapy may not work. This can be worrying, but just because one treatment hasn’t worked, it doesn’t mean others won’t.
Find out more about what happens when treatment doesn’t work.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.