Brain tumour seizure and epilepsy
A brain tumour might cause a seizure or epilepsy, which means having repeated seizures. This might happen because of the tumour creating a chemical imbalance in the brain, or causing the cells around the tumour to develop differently.

Short summary
Up to 2 in 3 people diagnosed with a brain tumour will experience epilepsy or at least one brain tumour seizure.
That may sound like a lot, but it’s important to remember that not everybody who is affected by a brain tumour will experience seizures or epilepsy.
For those that do, the symptoms and severity can be different for each person, so you might not have the same problems as someone with a similar diagnosis and treatment plan.
On this page:
- What are seizures and epilepsy?
- Brain tumour seizure symptoms
- What happens when I have a seizure?
- What causes seizures?
- Treating brain tumour-related seizures
- Coping with brain tumour-related seizures
- Frequently asked questions
Other symptoms
Use our Better Safe Than Tumour symptom checker to check for other brain tumour symptoms.
Talking to your doctor
Learn more about how to approach your GP.
Expert benefits & money advice
Benefits and Money Advice Clinic supported 339 people in the last financial year (22/23), to the tune of £807,938.
What is a seizure?
Our brains have billions of nerve cells which control the way we move, think and feel. They do this by passing electrical signals or messages to each other. So electrical activity is happening in our brains all the time.
A seizure happens when there’s a burst of abnormal electrical activity that disturbs the way the brain normally works, mixing up the messages. This causes a variety of symptoms.
Seizures are the most common first symptom leading to a brain tumour diagnosis in adults. However, you may only have seizures for a short period of time, for example, before treatment or due to swelling of the brain after surgery.
You’re more likely to have a seizure if:
- you have a slow-growing, low grade tumour
- if your tumour is in one of the lobes of the cerebrum (cerebral cortex) or the meninges (the membranes that cover and protect the brain and spinal cord).
What is epilepsy?
Epilepsy is the tendency to have repeated seizures, so it’s usually only diagnosed after you’ve had more than one seizure because of your brain tumour. There are more than 40 types of epilepsy of which brain tumour-related epilepsy (BTRE) is one.
Epilepsy caused by a brain tumour might be related to cells around the tumour that have developed abnormally. Or they may be due to an imbalance of chemicals in the brain caused by the tumour. Both of these can interfere with the normal electrical activity in the brain, leading to brain tumour epilepsy.
Brain tumour seizure symptoms
Brain tumour symptoms usually fall into one of two categories, being focal aware seizures and focal impaired awareness seizures. {anchor to below}
There are symptoms for each, which are:
Focal aware seizures
- feeling a bit spaced out or strange
- feeling very strong emotions for no particular reason
- sensing unusual tastes or smells
- feeling of ‘déjà vu’ (I’ve been here or done this before) or ‘jamais vu’ (familiar things seem new)
- feeling your stomach rise, as if you’re on a fairground ride
- muscle stiffness or twitching that can spread from the hand or foot and can affect half of the body
- feeling like you can’t speak, even though you’re fully conscious
- feeling tingling or numbness
- having a burning sensation
- feeling that an arm or leg is bigger or smaller than it is
- unusual things happening to your vision, like coloured or flashing lights
- seeing something that isn’t there (hallucinations).
Focal impaired awareness seizures
- trouble understanding or answering people, even though you can hear them
- if spoken loudly to, you may think the other person is being aggressive
- confused wandering
- language problems, such as comprehension
- making strange or repetitive movements or sounds (called ‘automatisms’)
- visual disturbances, like coloured or flashing lights
- hallucinations (seeing things that aren’t actually there).
What is likely to happen if I have a brain tumour seizure?
The effects of a seizure due to your brain tumour depend on:
If a seizure continues for more than 5 minutes or repeated seizures occur without recovery in between, emergency (rescue) medication should be given and an ambulance should be called immediately. Do not wait!
Types of seizures
When people think about seizures, they often think of convulsive seizures, where somebody loses consciousness, their body goes stiff and they fall to the floor with their limbs jerking.
Convulsive seizures are rarely experienced by people living with a brain tumour and sometimes referred to as fits – but are more correctly called tonic-clonic seizures.
However, there are many different types of seizures. They can range from convulsive seizure to absent seizures, where someone just feels a bit strange or spaced out.
Your seizures may not exactly match one of the types described, but they will usually last the same length of time and follow the same pattern each time they happen.
Seizures are grouped according to:
Where the seizure starts (the onset)
Focal onset (previously called partial seizures)
- Start in and only affect one part of the brain
- The most common type of seizures associated with brain tumours.
Focal to bilateral
- Start as a focal seizure, then spread to both sides of the brain.
Generalised onset
- Start in and affect both sides of the brain at the same time
- Start without warning
- These seizures are rarely associated with brain tumours, but when they do occur they are usually a type known as tonic-clonic.
Unknown onset
- The term for when it’s not known where in the brain they started, for example, if the person is asleep or alone and the seizure wasn’t witnessed.
Level of awareness during the seizure
Focal aware (previously called simple partial seizures)
- only a small part of one lobe of the brain is affected
- you’re fully aware, even if you can’t speak
- you remember the seizure afterwards, even if you can’t describe it.
Focal impaired awareness (previously called complex partial seizures)
- a larger part of one side of the brain is affected
- your consciousness is affected, so you may be confused or unaware of what you are doing
- you’re unlikely to remember the seizure afterwards
- you may feel tired afterwards.
Generalised seizures
- both sides of the brain are affected
- your awareness will affected in some way
- These seizures are rarely associated with brain tumours.
Whether your movement is affected
Motor seizures
- involve a change in your movement, for example, you pluck at your clothes or your muscles go stiff before making jerking movements.
Non-motor seizures
- there is no change in your movement, but there may be sensory effects, for example changes to your vision, smell or hearing.
Location in the brain
The effects of seizures or epilepsy which you’re likely to experience will also depend on where the tumour is in your brain and what that area of the brain controls. If your brain tumour is located over two different areas of the brain, you may experience a combination of seizure symptoms.
The following are examples of what can happen, but you may experience something different:
-
Focal aware
- an intense feeling of emotion
- an unusual smell or taste
- feeling of ‘déjà vu’ (I’ve been here or done this before)
- ‘jamais vu’ (familiar things seem new)
- rising feeling in the stomach, like you may get on a fairground ride.
Focal impaired awareness
- picking up or fiddling with objects or clothing
- chewing or lip-smacking movements
- uttering or saying repeated words that don’t make sense
- language problems, such as comprehension
- wandering around in a confused manner.
These may start as a focal aware seizure and usually last 2–3 minutes.
-
Focal aware
- muscle stiffness or twitching that can spread from the hand or foot and may affect half of the body
- feeling of not being able to speak despite being fully conscious.
Focal impaired awareness
- making strange movements or postures, such as cycling or kicking, usually at night
- screaming or crying out loudly or laughing uncontrollably.
These usually last 15–30 seconds.
-
Focal aware
- numbness or tingling
- burning sensation
- feeling that an arm or leg is bigger or smaller than it is.
Focal impaired awareness
- like the simple focal seizures in these lobes, these can affect your senses or vision.
These are less common than temporal or frontal lobe focal impaired awareness seizures and usually last 15–30 seconds.
-
Focal aware
- visual disturbances, such as coloured or flashing lights
- hallucinations (seeing something that isn’t there).
Focal impaired awareness
- like the focal aware seizures in this lobe, these can affect your
- senses or vision.
These are less common than temporal or frontal lobe focal impaired awareness seizures and usually last 15–30 seconds.
Status epilepticus
Occasionally, seizures may not stop, or one seizure follows another without any recovery in between. If this goes on for 30 minutes or more it is called ‘status epilepticus’ or ‘status’.
This is uncommon, but potentially serious, and requires hospital treatment. If you or a loved one is experiencing this, you should call 999 imediately.
What causes seizures and epilepsy?
Although epilepsy is more likely in certain low grade brain tumours, we don’t fully understand why this is the case.
Suggestions include abnormally developed cells around the brain tumour that fire (send signals) more often, causing disorganised electrical activity in the brain, which leads to seizures. This is sometimes the cause in people with non-brain tumour-related epilepsy.
Or it could be due to the tumour causing a disturbance in the balance of chemicals in the brain, causing the nerve cells to fire more often.
It’s important to remember that an increase in the frequency of your seizures doesn’t necessarily mean that your tumour has returned or is regrowing.
Treating brain tumour-related epilepsy
Treatment of seizures (epilepsy) in people living with a brain tumour can be particularly complex and difficult due to the additional effects that having a brain tumour causes. Treatments include:
- anti-epileptic drugs
- neurosurgery
- complementary therapies.
Depending on your diagnosis, some seizure treatments may not suitable for you or you may have to try several treatments before you find the one that is best for you.
Coping with brain tumour-related seizures
One of the ways to cope with seizures is to identify any particular triggers for you and lessen your exposure to them.
There are lots of strategies for making sure you’re as safe as possible when you do have a seizure or you’re better prepared to care for somebody who may experience seizures.
Join one of our Online Support Communities for more tips about coping with a brain tumour diagnosis, from people who truly understand what you’re going through.
Anxious about having a seizure?
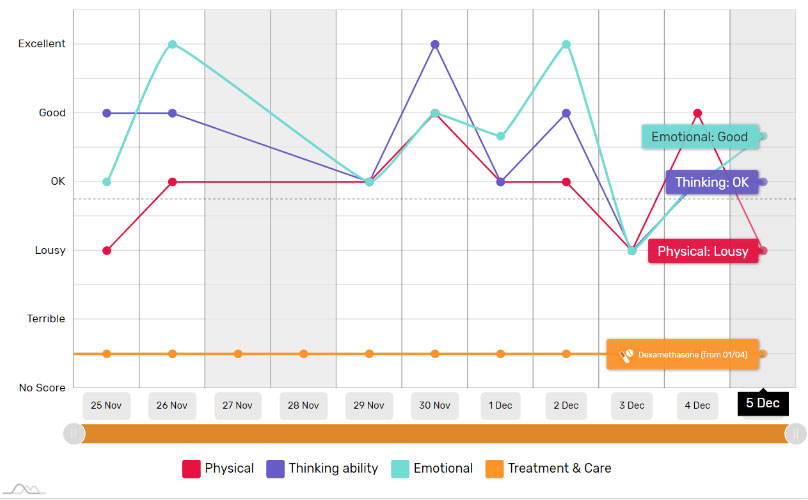
Not knowing when your brain tumour seizures might happen can make you feel insecure about being out in public or alone at home. Use BRIAN’s quality-of-life tracker to plot your seizures against possible triggers, so you can try to identify and avoid them.
Frequently asked questions
-
If you’ve been diagnosed with a brain tumour, you must tell the DVLA (DVA in Northern Ireland) as soon as possible.
If you’ve not yet given up your licence or you’ve had your licence returned after treatment, you must stop driving and tell the DVLA if you have a seizure of any type. This is a legal requirement.
Whether you can apply to have your licence returned will depend on various factors such as:
- the occurrence and type of seizures
- the restrictions applied because of your brain tumour.
-
If you’re the partner, family member or friend of someone recently diagnosed with brain tumour-related epilepsy, you may find yourself in the role of carer, particularly if their seizures are unpredictable or more severe.
It’s important you know what to do to keep them safe when they have a seizure, but this will depend on the type of seizure they’re having.
If a seizure continues for more than 5 minutes or occur repeatedly without time to recover in between, emergency (rescue) medication should be given and an ambulance should be called immediately.
Download our seizure factsheets
An introduction to seizures (epilepsy) and brain tumours – PDF
Find out more about seizures (epilepsy) and brain tumours – including more information about what happens during different seizures – in the full fact sheet.
Treatment for seizures (epilepsy) and brain tumours – PDF
Find out more about the treatment for seizures (epilepsy) and brain tumours, including ketogenic diet and cannabis-derived products.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.