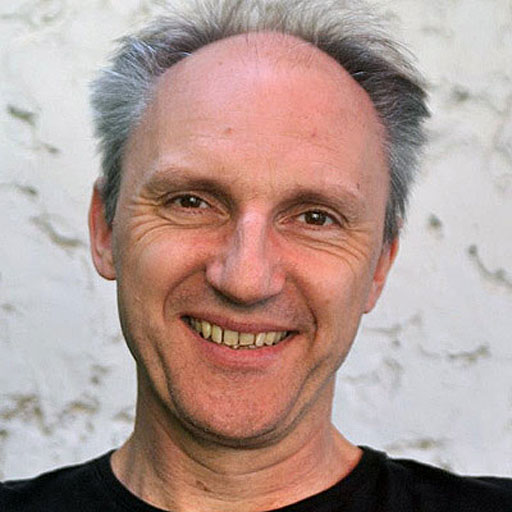
Q & A with Professor Sebastian Brandner
In the spring 2014 issue of The Grey Matters, our printed newsletter, we featured an interview with Professor Sebastian Brandner, one of the leading researchers we fund. You can read the full interview below.
Professor Brandner is Professor and Chair of Neuropathology at University College London. As well as conducting research, Professor Brandner is also a consultant clinical neuropathologist, working with his team to diagnose the type and grade of brain tumours by looking at a sample of tissue and carrying out molecular tests.
“Your fundraising is needed to establish centres of excellence to carry out high quality, internationally competitive research into brain tumours.”
Professor Sebastian Brandner
Why did you become a researcher?
I started my research career during Medical School in Göttingen, at the Max Planck Institute (MPI) of Biophysical Chemistry. Intrigued by the fascinating neuroscience research projects, which were at the time carried out at the MPI, I applied for a placement at the Neurobiology department where I carried out my research on the functional anatomy of the auditory system. This was very successful, resulting in several research publications as first author. Following the completion of medical school and after a placement in the Neurosurgical department at the University in Tubingen, I felt the desire to better understand the biology of brain tumours.
I joined the Department of Neuropathology at the University Hospital in Zurich, which at the time was led by Prof Kleihues, the co-founder of the WHO classification of brain tumours and an active and highly renowned brain cancer researcher. Whilst I carried out highly successful prion research with Prof Aguzzi, I still wanted to pursue experimental brain tumour research. Intrigued by the biology and pathology of brain tumours, I established my own research group and developed innovative models to study neural development and brain tumours. In 2001, I was recruited through the MRC international recruitment scheme to the UCL Institute of Neurology and in 2004 I was appointed as Chair of Neuropathology and Head of the Division of Neuropathology at Queen Square, one of the largest academic neuropathology departments in the UK.
My research on brain tumours resulted in multiple high profile publications in Development, EMBO Journal and Cancer Research, showing how stem and progenitor cells of the adult brain can give rise to brain tumours and how these tumours relate to human disease. I have developed a major team working on brain cancer and established close collaborations between UCL Cancer Centre and the Brain Tumour Unit at the National Hospital.
Can you give us an idea of your typical day?
My typical day often starts with a clinical multidisciplinary meeting where for example we discuss the diagnoses of brain tumour patients. On other weekdays, we start with a departmental diagnostic review meeting to peer-review our diagnoses. This serves quality control and also keeps all consultants and trainees informed about rare, or difficult cases. Typically I would before lunchtime have a meeting with my students, postdocs or technicians to be updated on the progress of projects. Once a week my research team meets and we discuss relevant literature and new experimental data.
One in three or four weeks I am in charge (in rotation with other consultants for the other weeks) of all biopsies coming from our hospital. I would then be on call to diagnose intraoperative sections, and at midday I meet with my trainees at our departmental multiheader to diagnose all brain tumour cases that are sent from the theatres in the National Hospital next door. Thirty to 50% of brain tumours are reported within 24 hours. Only 2% of our cases need more than 5 working days to be reported. This is important for the clinical teams, in order to tell the patients the diagnosis as soon as possible, and to either discharge them or to start adjuvant treatment as quickly as possible.
Often I have in the afternoon meetings with visitors, researchers, finance managers, senior laboratory personnel, or I do for example appraisals of our staff or I sit on committees. After 5pm when there are no more meetings and no disruptions I work on scientific publications or on other documents, for example, guidelines or educational material, or I prepare for lectures.
What do you hope your research project will achieve?
One of the key goals is to increase the understanding of the pathogenesis of brain tumours. This specific project looks into the role of a mutant enzyme, IDH1 which was discovered 5 years ago to be a characteristic mutation in astrocytic and oligodendroglial tumours. Yet, it is still not clear how this mutation can actually lead to a brain tumour. We establish here a model of brain tumours that carry an IDH1 mutation which is identical to that in 70% of primary human astrocytomas and oligodendrogliomas. Currently we compare the IDH1 mutant brain tumours generated in this model with existing, well-characterised and validated model systems.
We also address the essential question, if IDH1 mutations are indeed glioma initiating events, as it is currently claimed for the pathogenesis of human gliomas. We hope that we can use this model to understand from which cells these tumours arise and if other mutations are needed to cause a brain tumour. This will be achieved in a genetically engineered model, in which we can in stem cells switch on mutant IDH1. We will then compare these new tumours with those from earlier experiments.
Such a model will have patient benefit in that it can be used as a pre-clinical model to test drugs that can help suppress the growth of cells with such mutations.
How far can research into brain tumours move forward in the coming years?
There has been significant progress made in the understanding of clinical subgroups of medulloblastoma. Tumours such as glioblastoma would benefit from progress even in a small subgroup. Some subclasses have already been identified and it is possible that continuous, tenacious focus on the biology of these tumours may result in a significant success for a small but clearly defined subgroups of patients with such tumours.
Why is more money needed for research into brain tumours?
The incidence and the deaths from brain cancer are rising, unlike most other cancers. Incidence went up by approximately 25% and deaths more than 10% since 1970, but less than one in five of those diagnosed with a brain tumour survive beyond five years, compared with an average of 50% across all cancers. Nearly two thirds of men and women diagnosed with brain cancer die within a year compared to 35% for leukaemia, 7% for prostate cancer and 5% for breast cancer.
The demographics of brain cancer indicate that more children and adults under 40 die of a brain tumour than from any other cancer and three in four brain tumour deaths occur in those under 75 compared to just half of deaths for all other cancers. 16,000 people each year are diagnosed with a brain tumour.
Brain tumour research is underfunded and treatments fall back seriously behind other cancers. Less than 1% of the national spend on cancer research goes to brain cancer. Our understanding of other cancers does not readily translate to brain tumours and thus much more research is needed to discover the cause of brain tumours and to understand their pathobiology and natural history.
What would be your message to anyone thinking about fundraising for The Brain Tumour Charity?
Your fundraising is needed to establish centres of excellence to carry out high quality, internationally competitive research into brain tumours.
It is also fundemental to boosting research in already established centres or groups with a proven track record of research excellence, and to give these groups much-needed continuity in funding, which is essential to maintain momentum, retain highly skilled researchers in a research team and to bridge funding gaps to complete high quality publications.