Paediatric research update
Our research is attacking childhood brain tumours on all fronts. We’re improving understanding of brain tumours in the lab, we’re getting the most cutting edge techniques into clinical trials and we’re helping families affected by these tumours build a brighter future.

Our research is helping to reduce aggressive treatments without impacting survival and we are striving to improve on this with every paediatric grant we fund.
We’re excited to share the latest progress from a selection of those grants below. At the end of each progress update you’ll find the link to the grant’s own webpage where you’ll find more information.
Origins of medulloblastoma
Lead researcher: Dr Laure Bihannic
Where: St Jude Children’s Research Hospital, Memphis USA
Cost: £180,000 over three years, initially
Dr Laure Bihannic started this three-year grant in September 2018. This grant was awarded as part of our Future Leaders funding, which has the overall aim of growing the field of researchers working on brain tumours and ultimately bringing them to the UK. In line with this she will be eligible to apply for further funding at the end of her current grant.
Cell of origin
Dr Bihannic has studied cerebellar development using a new technology known as single-cell RNA sequencing. This approach identified individual cerebellar cell types present during the development of the murine cerebellum. She then studied patient MB using the same technique (i.e. single-cell RNA sequencing).
By comparing the tumour cells and the developing cerebellar cells she identified two cell populations as highly similar to Group 4 medulloblastoma. These cell types are glutamatergic cerebellar nuclei (GluCN) and unipolar brush cells (UBCs), suggesting that they might be the cells from which Group 4 tumours originate. They will now isolate these cells in their models to study them in more depth.
Functional validation of medulloblastoma subgroup origins
The goal of the work above is to determine the normal cerebellar cell populations most similar to human tumour counterparts. These efforts, although necessary, will be insufficient to definitively prove cellular origin without direct functional evidence. After proposing the subtype-specific cell of origin, Dr Bihannic will endeavour to grow them in the lab in a way that mimics the childhood disease.
Her future studies will disturb the Group 4 medulloblastoma candidate populations, GluCN and UBCs, by overexpressing genes that have been implicated in Group 4 medulloblastoma formation. The ultimate aim would be to prove these cells cause tumours by implanting them in pre-clinical models and monitoring them for signs of tumour initiation.
Targeting ALK2 inhibitors for DMG (formerly known as DIPG)
Lead researcher: Dr Alex Bullock
Where: Structural Genomics Consortium, Oxford
Cost: £491,051 over four years
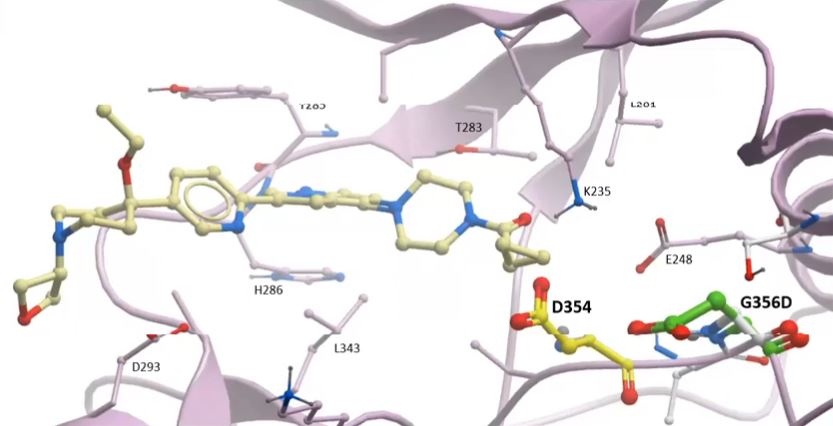
To date, the research has produced about 400 chemicals that have potential as DMG drugs. In Oxford, researchers have tested these the lab to assess:
- how tightly they bind to the intended target, the ALK2 protein;
- whether they do this specifically (desirable) or bind equally to other proteins which may cause toxicity; and
- how well they kill DIPG cells.
Progress is shared regularly at monthly team meetings which are recorded and shared on YouTube as well as through a blog with a lab notebook.
Click to view the latest progress video.
Most encouragingly, Dr Bullock’s team have identified a group of potential drugs that bind strongly to ALK2 and cause patient-derived DMG cells to grow more slowly. From these, the researchers will focus on five top drug candidates that will be further investigated with the ultimate aim of getting them into clinical trials.
Since this project started the research has been going so well that the researchers have set up a new company, called Meds4Kids, to drive the potential drugs through the next stage of development and on to clinical trials.
ACP research and an upcoming clinical trial
Lead researcher: Dr Todd Hankinson
Where: University of Colorado, USA
Cost: £1.058 million over five years
Adamantinomatous craniopharyngioma (ACP) is a low grade brain tumour usually found in children. It has a profound effect on children’s quality of life due to the location of the tumour – near the pituitary gland, hypothalamus and optic nerve.
Previous research has shown that the different types of cells that make up ACPs communicate with each other using chemical messengers called cytokines. Cytokines are molecules released from cells that allow them to ‘talk’ to each other and promote survival and growth. Researchers suspect that in ACP these chemical messengers are promoting tumour growth but we need to know more.
Understanding how ACP cells communicate
Dr Hankinson and his team have refined the technique they will are using to separate out the individual cells within the tumours. They’re now using ethically-donated human ACP samples to find which cell types are producing different cytokines.
Identifying treatments for ACP
When the research team know which cytokines are involved they are able test the best potential drugs in pre-clinical models. The team are now analysing the experiments they did using the first of their candidate drugs.
Once the researchers confirm that one or more drugs are reaching the tumour in effective levels they will ask the questions, ‘Are the drugs killing the tumour?’ and ‘Which ones are doing it best?’
Doing research on uncommon tumours is very difficult to do and having multi-national and multi-institutional support is very hard to find. The support provided by The Charity is critical to accelerate progress.
Dr Todd Hankinson
Testing treatments in the clinic
From our perspective, this is the most exciting progress in the grant because it’s been accelerated beyond what we thought the grant would produce.
The researchers have been able to advance their timetable and we’re now funding their Phase II trial instead. (Phase I trials aren’t needed in this case because the drugs have already been tested for safety).
Phase II trial: A panel of experts from the CONNECT consortium assessed the data our researchers provided and accepted their proposal for treating children with an immunosuppressive drug alongside a type of drug called a MEK inhibitor. This shows how the work is racing towards the clinic.
The Everest Centre
Lead researcher: Dr David Jones
Where: German Cancer Research Centre (DKFZ), Germany
Cost: £5 million over 5 years, initially
The team funded by The Everest Centre grant is making great progress towards their objectives. Under the leadership of Dr David Jones, they’re advancing their work into the epidemiology, genetics and molecular biology of low grade paediatric brain tumours, and the clinical trial that’s supported by this grant, LOGGIC, is already gathering data.
Determining the origin of low grade brain tumour types
The team have defined two new subtypes of low grade brain tumour, which were previously only poorly characterised. Both new subtypes have unusual features in terms of their genetic alterations, making them somewhat different from other low grade tumours. This is interesting biologically and also important for developing targeted treatment strategies in the future.
Developing low grade brain tumour models and pre-clinical screening
Further progress on this aim has seen development of the tool that allows the researchers to track activity of key signalling molecules within the cells in real-time. They’re now using this system to screen large panels of drugs with the ultimate goal of finding combinations of treatments that more effectively switch off the main tumour-driving proteins in the cell.
Identifying factors that affect tumour growth
In London, the team has generated a large amount of data on two distinct types of low grade brain tumour, as well as normal brain tissue for comparison. In contrast to previous data on the DNA and RNA components of the tumour cell, they’re now examining the proteins and protein activity within the cell directly. This data will be extremely useful for detailing how key cancer pathways are activated within the cells and prioritising areas for further study in tumour models.
Enabling a pan-European clinical trial, called LOGGIC (LOw Grade Glioma In Children)
The first phase of the study, the LOGGIC Core BioClinical Database, is now open and collecting information on newly-diagnosed patients as well as providing detailed molecular analysis of their tumours. So far, more than 80 patients in Germany are registered, and the molecular screening has already revealed some unexpected findings that will help to provide more accurate diagnosis (as well as offering potential treatment options). This part of the study is currently being opened up in additional international hubs, including the UK, and we expect the full clinical trial to start in early 2020.
Clinical impact
Pathologist Professor Thomas Jacques, along with other Everest researchers in the UK and Germany, examined the clinical value of performing routine molecular testing in childhood brain tumour patients to assist with diagnosis. They found that in cases with an unusual appearance under the microscope, or showing uncommon clinical behaviour, the use of these molecular tools (originally developed by Everest researchers in Heidelberg) could greatly help in providing an extra degree of diagnostic certainty. Sometimes even suggesting more effective treatments. Read more about this exciting clinical development.