Chemotherapy for brain tumours
Chemotherapy is a type of treatment that uses tumour-fighting drugs to fight brain tumour cells. These anti-cancer drugs are circulated through your body in your bloodstream. Chemotherapy can be used as a treatment on its own, or it may be used with or after surgery or radiotherapy.
On this page, we’ll discuss:
What is chemotherapy?
Chemotherapy is the use of anti-cancer (cytotoxic) drugs to destroy tumour cells. These drugs interfere with the way tumour cells divide and create copies of themselves, causing them to die.
Chemotherapy also affects healthy cells, but they’re able to repair themselves better than tumour cells. This means fewer heathy cells die after treatment.
Chemotherapy drugs are generally absorbed or injected into your bloodstream and carried around your body to reach the tumour cells. Sometimes they’re put directly into the brain or cerebrospinal fluid (CSF) that surrounds the brain.
How is chemotherapy for a brain tumour given?
There are various ways that chemotherapy can be given, and your healthcare team will decide which is best for you:
-
These are taken much like any other tablet, so you can take the tablets at home.
However, you should take care to touch the tablets/capsules as little as possible and should wash your hands straight afterwards.
Other people in your household should avoid touching them at all. If someone has to give you your tablets/capsules, they should use clean (washed) rubber or disposable gloves, AND wash their hands afterwards. If possible, they should not handle the chemotherapy drugs if they’re pregnant or breastfeeding.
You should not crush or cut your tablets, nor open your capsules, unless you’re advised to.
There can be an after-taste to these drugs – chewing flavoured gum afterwards can help to disguise this taste.
As with all medication, tablets should be kept out of the reach of children.
-
Chemotherapy drugs can be injected into a vein (intravenously) or into the cerebrospinal fluid around the spine (intrathecally).
When given intravenously, they may be given via a drip into your vein. This takes from over half an hour to a few hours, and will be done in hospital, but usually as an out-patient.
-
The chemotherapy drug carmustine is sometimes added to a biodegradable wafer, called a Gliadel® wafer, and put into the brain during surgery. Placed in the area the tumour has been removed from, they’re used to target cells which couldn’t be removed by surgery.
As the wafers are biodegradable, they gradually dissolve over 2-3 weeks, releasing the chemotherapy drug directly into the brain. This has the advantage of getting around the blood-brain barrier, which prevents many drugs entering the brain.
It’s important to note that Gliadel® wafers are only licensed for high grade gliomas where at least 90% of the tumour has been removed by surgery. Their suitability for use also depends on where the tumour is in your brain.
They may also cause some side-effects, such as seizures, swelling in the brain and delays in wound healing from the surgery.
-
This is a dome-shaped device that is put under the scalp during an operation. It delivers chemotherapy directly into the cerebrospinal fluid (CSF), which delivers the drug directly to the brain, increasing its effectiveness.
However, giving chemotherapy this way can be complicated and difficult, so it isn’t routine treatment for most people with a brain tumour.
What to expect from chemotherapy
Before chemotherapy is given
Your healthcare team will carefully consider the best course of treatment for you. This will depend on:
- the type of tumour you have and whether it has spread within the brain
- your general health and fitness
- your age.
Your healthcare team will also explain why you’re having chemotherapy. This could be:
- during or after surgery, to control cells that haven’t been removed and so delay or reduce the chance of the tumour returning
- with or after radiotherapy, to reduce the risk of tumour regrowth
- to treat a tumour that’s returned
- to shrink or control a tumour that can’t be operated on
- to prevent or slow further growth of a tumour.
Asking questions
Your healthcare team will also talk through what will happen and discuss any potential chemotherapy side-effects with you before any treatment is given.
This is your chance to ask any questions. Remember, no question is a silly question.
Helping you prepare for chemotherapy
Would you like to receive our four-part email guide to your treatment?
During chemotherapy
You’ll be given chemotherapy in a series of treatments separated by rest periods. One treatment session and rest period is called a ‘cycle’ and a number of cycles make up the ‘course’ of treatment.
As well as your chemotherapy sessions, you’ll have regular blood tests to check your blood cell count is satisfactory. Chemotherapy can affect your blood cell production which can lead to serious side-effects.
And you’ll usually be scanned every 3 months during treatment to see if the treatment is having an effect.
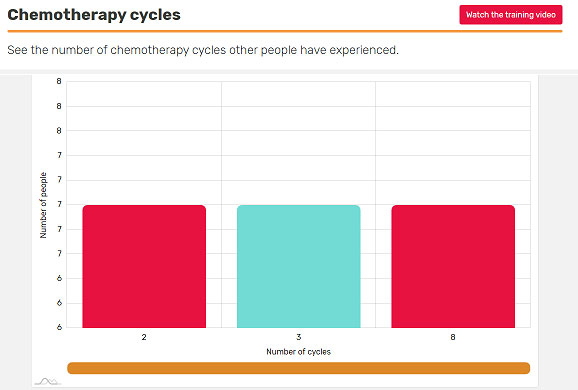
How many cycles of chemotherapy can you expect?
If you’re about to have chemotherapy, or you’ve been told you’re not having it, you may wonder if this is usual in your situation. Find out with BRIAN’s Chemotherapy cycles insight, which you can filter to make it relevant to you.
After chemotherapy
After you start having chemotherapy, you may experience a variety of side-effects.
Because chemotherapy affects rapidly or frequently dividing cells, any healthy cells in the body that divide frequently are also vulnerable during chemotherapy. These include skin and hair cells and those lining the digestive system.
Although treatment plans are carefully developed by healthcare professionals to be as effective as possible, while having the fewest risks or side-effects, sometimes chemotherapy may not work.
If chemotherapy doesn’t work
This can be worrying, but just because one treatment hasn’t worked, it doesn’t mean others won’t.
Frequently asked questions
-
Individual treatment plans vary and yours will be carefully planned specifically for you. Typically a course of treatment may last 6-12 months, consisting of 6-12 cycles. You may have chemotherapy for a few days, every few weeks.
-
Chemotherapy is generally given as an outpatient treatment, which means that you don’t have to stay in hospital overnight, although in certain circumstances you will need to. Your healthcare team will talk to you about this before you start your treatment.
-
Depending on the hours you work, you will probably need to arrange time off for hospital appointments. Side-effects, such as tiredness and nausea, may mean you need a longer period of time off work.
Our employment resources provide help and information on how to approach your employer about your diagnosis and how they can support you through this time.
-
You’ll have regular check-up appointments following treatment, which will sometimes include scans. These appointments may continue for a number of years after your chemotherapy has finished.
-
You’ll be monitored for any changes to the tumour, sometimes during and sometimes following treatment. This can be through the use of MRI and CT scans to see whether the tumour is shrinking.
By joining one of our Online Support Communities, you can get more tips about living with or beyond a brain tumour diagnosis from people who truly understand what you’re going through.
More information
Chemotherapy for adults factsheet – PDF
Find out more about chemotherapy for adults in the full fact sheet – including side-effects and links to information about wigs and head coverings.
Chemotherapy for adults – Clear print factsheet – PDF
Find out more about chemotherapy for adults in the full fact sheet – Clear print version, designed to RNIB standards. This includes side-effects and links to information about wigs and head coverings.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.