Neurosurgery for brain tumours
Neurosurgery is surgery that’s done on the brain or spinal cord. It’s one of the main treatments for brain tumours, and is often the first.
Neurosurgery carried out by a highly specialised doctor called a neurosurgeon. Every hospital or surgeon may have slightly different practices, so what you experience may differ a little from what’s described below or from what other people experience.
On this page:
What is neurosurgery?
Neurosurgery is surgery performed on the brain or spinal cord.
For brain tumours, neurosurgery can be performed to:
- remove all or part of the tumour
- diagnose your tumour type, known as a biopsy
- put chemotherapy drugs directly into the brain
- put in a device, called a shunt, or create a bypass to reduce the build-up of the cerebrospinal fluid.
It’s important to know that neurosurgery is not always possible. If your brain tumour is too close to an important part of your brain, surgery may be too risky.
In this case, another treatment option will be suggested by your healthcare team.
Types of neurosurgery
There are two main types of neurosurgery. These are:
Craniotomy
A craniotomy is when the surgeon makes an incision into the scalp and removes a piece of bone from the skull. This allows them to remove as much of the brain tumour as possible.
A craniotomy is the most common type of surgery for a brain tumour.
Neuroendoscopy
Often called keyhole surgery, neuroendoscopy is a less invasive type of surgery. It is used to reach parts of the brain that might not accessible through a craniotomy, and is also valuable in that it means less of the skull needs to be cut.
During a neuroendoscopy, a surgeon will cut a small hole in the skull and insert and endoscope. This is a long instrument with a camera on its end, allowing the surgeon to see inside the skull. The surgeon then uses the small scissors (called forceps) at the tip of the endoscope to remove as much of the tumour as possible.
Neuroendoscopy usually results in faster healing and less scarring than a craniotomy.
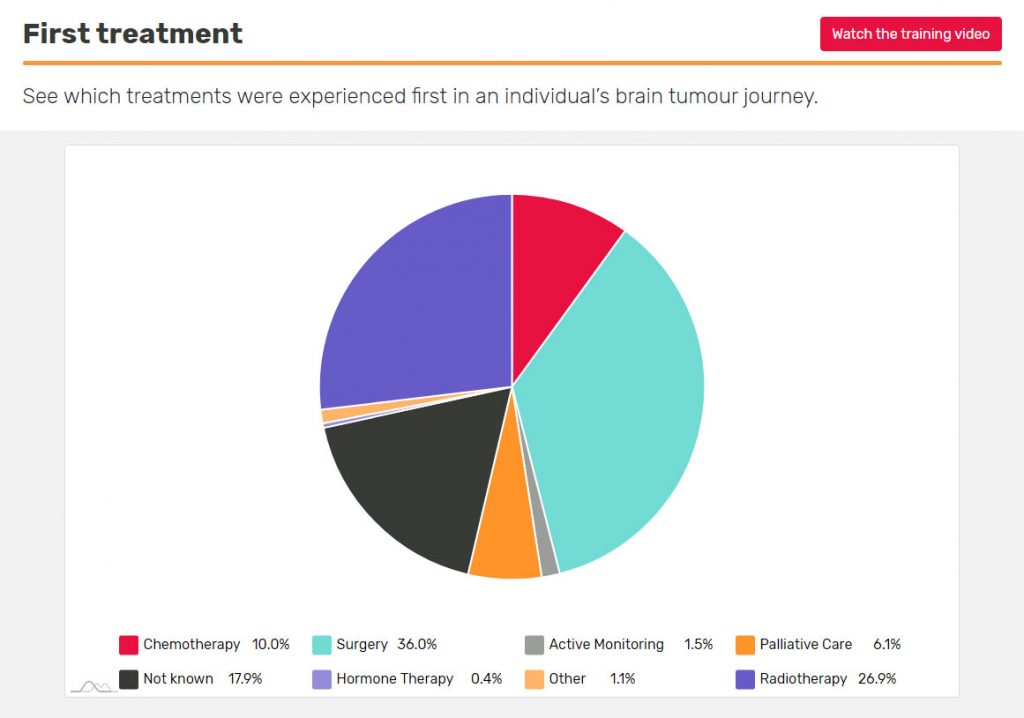
What treatment do people with a similar diagnosis have first?
If you’ve just been diagnosed and are about to have treatment, you may want to see what other people’s first treatment was. Use the First Treatment insight in BRIAN, which you can personalise to make it relevant to you.
What to expect from neurosurgery
Before neurosurgery
This is the time when your healthcare team will explain your surgery.
Use this time to ask as many questions as you want. There’s no such thing as a silly question. It’s better that you ask and have things explained, than worry about them.
Neurosurgical Outcomes Data
In planning for your surgery you may wish to know more about who you are being seen by or seek a second opinion. The NHS website has information about consultants specialising in neurosurgery in England, along with some data concerning their neurosurgical outcomes.
When looking at this information, it’s important to remember that statistics aren’t always able to show other factors that may affect the outcomes. For example, some surgeons may have lower survival rates as they’re willing to take on more complex cases.
During neurosurgery
Your treatment will be different depending on the reason you’re having neurosurgery. Find out more about what happens during the surgery you’re having by clicking the links below:
- craniotomy to remove all or part of the tumour
- a biopsy to diagnose the type of tumour you have
- delivering chemotherapy drugs directly into the brain
- putting in a shunt to reduce the build-up of the cerebrospinal fluid
Helping you prepare for surgery
Would you like to receive our five-part email guide to your treatment?
After neurosurgery
Immediate effects
Some people wake up quickly after neurosurgery, while others may take a few hours or days.
Find out more about what to expect when you first wake up and temporary short-term side-effects of neurosurgery.
Going home after brain tumour surgery
Going home after brain tumour surgery can also be a nervous time. Find out more information about common symptoms you may continue to have, symptoms that require medical attention, and answers to frequently asked questions around medications and practical issues, such as washing your hair.
Follow-on treatment
After a few days, you’re likely to have a brain scan to see how much, if any, of the tumour remains and how much swelling you have.
You may be given:
- steroids to reduce swelling and pressure on the brain
- anti-epileptic medication to try and prevent seizures due to increased pressure in the head.
You may then be given chemotherapy, radiotherapy or both, to get rid of any remaining tumour cells.
You’re likely to have regular scans in the weeks/months after surgery. Initially these will be done more frequently, then the time between them may become longer. Your healthcare team will let you know about the scans you need, as this will depend on your tumour type.
By joining one of our Online Support Communities, you can get more tips about living with or beyond a brain tumour diagnosis from people who truly understand what you’re going through.
If neurosurgery doesn’t work
Although treatment plans are carefully developed by healthcare professionals to be as effective as possible while having the fewest risks or side-effects, sometimes neurosurgery may not work. This can be worrying, but just because one treatment hasn’t worked, it doesn’t mean others won’t.
Frequently asked questions
-
You will have to take some time off work for treatment and for some time afterwards to recover. Side-effects, such as tiredness, nausea or cognitive difficulties, may mean you need a longer period of time off work.
Our employment resources provide help and information on how to approach your employer about your diagnosis and treatment effects, and how they can support you through this time.
-
A biopsy is a sample of tumour tissue removed during neurosurgery. This is primarily used for diagnosis, to find out what type of brain tumour you have. This is done by sending the tumour sample to a lab where its biomarkers and characteristics are analysed.
If, after testing to establish diagnosis, there is tumour tissue left, it may be stored in a tissue bank for use in the future. Tumour tissue can be used for research purposes (e.g. the Tessa Jowell Brain MATRIX study) and could also be used in future and emerging novel treatments, such as cancer vaccines.
How a tissue sample can be used depends on the amount that is obtained during neurosurgery and also how it is stored.
The standard method for storing tissue is known as formalin fixation and paraffin embedding (FFPE). However, this can cause some damage to the genetic material in the sample and make future use limited.
Flash freezing is another type of tissue storage which is better at preserving the tissue. Having your tumour sample flash frozen may mean you are eligible to access specific clinical trials or future and emerging treatments.
The British Neuro-oncology Society (BNOS) have written some guidelines for the tissue sampling of brain tumours.
Ask your neurosurgeon whether flash freezing could be possible for you. Brainstrust have an information sheet on talking to your neurosurgeon about tissue collection.
Neurosurgery (adults) – (pdf) –
Find out more about Neurosurgery for adults in the full fact sheet – including longer-term effects and information about when you can return to activities, such as sport or flying.
Neurosurgery (adults) – Clear print (pdf) –
Find out more about Neurosurgery for adults in the full fact sheet – including longer-term effects and information about when you can return to activities, such as sport or flying. Clear print version, designed to RNIB standards.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading

What happens before and after neurosurgery?
Stuart Smith, Neurosurgeon and Clinical Associate Professor at The University of Nottingham explains what patients can expect when they have neurosurgery, both before and after the operation.
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.